Holiday weekends can place added strain on labor and delivery units. At the same time, childbirth does not pause for staffing schedules, vacations, or rotating coverage. Labor can shift quickly from routine to critical, and fetal monitoring often provides the first warning that something is wrong. When hospitals operate with reduced staff or rely heavily on shift changes during holiday weekends, important fetal monitoring red flags can be overlooked or acted on too late.
Understanding how these breakdowns occur can help families recognize when a birth injury may have been preventable and why further review may be necessary.
How Fetal Monitoring Protects Babies During Labor
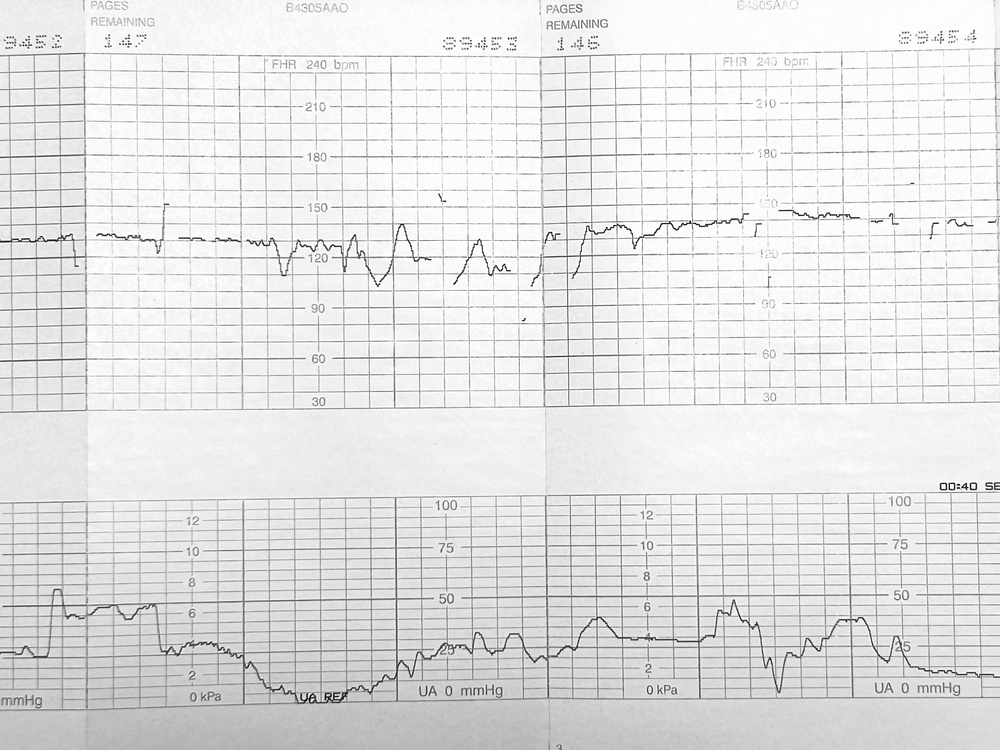
Fetal heart rate monitoring allows clinicians to assess how a baby responds to contractions and stress during labor. The monitor tracks baseline heart rate, variability, accelerations, and decelerations. Together, these patterns help indicate whether a baby is receiving enough oxygen.
Monitoring alone does not prevent injury. Safety depends on continuous interpretation, documentation, and timely intervention. When staffing is stretched or communication breaks down, warning signs can go unnoticed or minimized.
Fetal Monitoring Red Flags That Require Attention
Some fetal heart rate changes are temporary and resolve with basic interventions. Others signal a developing emergency that requires prompt escalation.
Common red flags include:
- Minimal or absent variability lasting more than a brief period
- Recurrent late decelerations following contractions
- Recurrent variable decelerations with slow recovery
- Prolonged decelerations lasting several minutes
- Sustained bradycardia or tachycardia
- A sudden shift from reassuring to nonreassuring patterns
The key factor is persistence. When concerning patterns continue or worsen over time, delay can increase the risk of hypoxic injury.
Why Holiday Weekends Increase Risk In Labor And Delivery
Hospitals often anticipate lower staffing needs during holidays. However, labor volume does not always drop, and emergencies still occur. Holiday weekends can introduce several risk factors at once.
Units may rely on skeleton crews, on call physicians, or staff covering unfamiliar assignments. In addition, fewer specialists may be immediately available, which can slow escalation and decision making.
Even experienced clinicians can struggle when responsible for too many patients at once. As workloads increase, bedside monitoring can decrease.
How Understaffing Leads To Missed Red Flags
Understaffing rarely causes harm through one obvious mistake. Instead, it creates conditions where small delays accumulate.
A nurse may notice a subtle change but become distracted by another patient. A physician may not be notified immediately because staff assume the issue will resolve. Monitoring strips may not be reviewed closely for trends over time.
When fewer nurses are available, continuous reassessment becomes harder. This matters because fetal distress often develops gradually, not suddenly.
Documentation can also suffer. Late or incomplete charting may obscure when a problem began, how long it lasted, and what interventions occurred.
Shift Changes And Communication Gaps
Shift changes are a known vulnerability in hospital care. During holiday weekends, handoffs may occur more frequently due to rotating coverage, overtime limits, or staffing substitutions.
Effective handoffs require clear communication about fetal monitoring trends, recent changes, and contingency plans. When these details are rushed or omitted, the incoming team may assume stability that does not exist.
Common handoff failures include:
- Summarizing the strip instead of reviewing trends
- Failing to mention recent medication adjustments
- Not clarifying who contacts the physician if patterns worsen
- Assigning too many patients to incoming staff at once
These gaps can delay recognition of a deteriorating fetal condition.
Similar Post: Can Preventable Birth Injury Deaths Be Avoided With Better Protocols?
Medications And Interventions That Demand Close Monitoring
Certain labor interventions increase the need for vigilant monitoring. Pitocin can intensify contractions, which may reduce oxygen delivery between contractions. Epidurals can affect blood pressure and uterine blood flow if not managed carefully.
During holiday staffing shortages, reassessments may be delayed. Central monitoring stations may replace bedside checks, even though artifacts or signal loss can hide changes.
When staffing is adequate, clinicians can reposition sensors, confirm readings, and ask for second opinions. When staffing is thin, borderline tracings may not receive the attention they require.
What Timely Escalation Should Look Like
When fetal monitoring shows persistent nonreassuring patterns, the standard response includes prompt evaluation, corrective measures, and escalation if the tracing does not improve.
This may involve medication adjustments, additional monitoring, physician assessment, or operative delivery. The goal is to prevent prolonged oxygen deprivation.
Delays during holidays can mean waiting for available providers, operating rooms, or anesthesia teams. Each delay increases the risk of permanent injury.
What Parents Often Observe During Overwhelmed Shifts
Parents may not understand fetal monitoring terminology, but they often notice warning signs in real time. These include long periods without bedside checks, alarms that go unanswered, frequent staff changes, and unclear explanations.
While these observations alone do not prove negligence, they often align with documentation gaps found later in medical records.
What Families Can Do If Concerns Arise
If a baby required resuscitation, NICU admission, cooling therapy, or treatment for seizures, families can take steps to preserve important information.
These steps include:
- Requesting the full medical record, including fetal monitoring strips
- Writing a detailed timeline of labor and delivery events
- Saving neonatal diagnoses, discharge summaries, and follow up plans
These records can help determine whether fetal monitoring red flags were missed or ignored.
Similar Post: What Happens When Your Hospital Is Short-Staffed During Winter and Your Baby Is Harmed?
Why Missed Red Flags Matter In Birth Injury Claims
Birth injury cases often focus on timing. The central question is whether the care team recognized distress early enough and acted appropriately.
Holiday staffing issues do not excuse delayed care. Hospitals have a duty to anticipate predictable risks and maintain safe coverage.
When missed monitoring leads to preventable injury, families may have legal options worth exploring.
Speak With Anapol Weiss About Birth Injury Concerns
If you believe missed fetal monitoring red flags during a holiday weekend contributed to your child’s injury, Anapol Weiss can review the medical records and help you understand your options. The firm evaluates whether staffing shortages, shift changes, or delayed responses played a role in what happened.
You can call 866-944-0553or submit an online contact form to schedule a free consultation and discuss your concerns with a team that understands the medical and legal complexities of birth injury cases. We represent families throughout the country, including Manayunk, Old City, Rittenhouse Square and elsewhere in Philadelphia County.
Disclaimer: This blog is intended for informational purposes only and does not establish an attorney-client relationship. It should not be considered as legal advice. For personalized legal assistance, please consult our team directly.
